An estimated
In fact, most of us probably know someone who has been affected by cancer.
Indeed, it is hard to think of a condition more well known than cancer. Although many medical terms remain obscure, “cancer” has adopted a new meaning in common parlance: “something evil or malignant that spreads destructively.”
Although cancer is still a leading cause of death globally, scientists continue to make advances in the prevention and treatment of this condition.
Looking back just a few decades, people often advised young scientists and doctors against following a career in oncology because of its complexity and the discouraging clinical outcomes.
This is no longer the case, as the authors of one paper note:
“Today, oncology is one of the most exciting fields in biomedicine because of the many astonishing advances research continues to yield.”
To celebrate some of the advances that oncologists are making, we contacted researchers from a number of institutions. We asked them to share recent findings that excite them. Here, we provide a sneak peek at what’s new in cancer research in 2021.
Article highlights:
Focus on the centrosome
First, we heard from Prof. Steve Royle. Prof. Royle is affiliated with Warwick Medical School at the University of Warwick in the United Kingdom.
“As a cell biologist, I am interested in the changes in normal cells that lead to cancer. A recent paper from Susana Godinho’s lab at Bart’s Cancer Institute in London, U.K., caught my eye.” The study in question investigated the role of a particular organelle: the centrosome.
In healthy cells, there is just one centrosome. It plays a pivotal role in the regulation of cell division. As part of the cytoskeleton, it also provides the cell with structure.
Scientists have known for some time that certain types of cancer cells have
Prof. Royle explained the recent study, saying: “The authors found that cells with too many centrosomes […] secrete tiny packets called small extracellular vesicles. It seems that these packets are a way for the cancer cell to communicate with the surrounding tissue. In pancreatic cancer, the ‘message’ from these packets favors cancer cell movement.”
The authors of the paper, which now appears in the journal
“Our findings demonstrate that centrosome amplification promotes quantitative and qualitative changes in secreted [small extracellular vesicles] that could influence communication between the tumor and the associated stroma to promote malignancy.”
As Prof. Royle explained, “The process by which cancer cells move and invade healthy tissue is of huge interest because this is the way that metastases occur, the most dangerous aspect of cancer.”
He is hopeful that understanding this mechanism could lead to novel treatments in the future.
Immunotherapies
Dan Kitwood/Getty Images
“What am I excited about? Immunotherapies,” said Prof. Mark Middleton, head of the Department of Oncology at the University of Oxford in the U.K.
Immunotherapy is a relatively new approach to treating cancer. In a nutshell, immunotherapy helps the body’s immune system recognize and attack cancer cells.
“Immunotherapies, such as the Oxford-developed tebentafusp, open up a whole
Prof. Middleton also believes that “multidisciplinary projects are the future of cancer research.”
“For example,” he said, “we are working alongside engineering researchers in our PanDox trial to improve drug delivery.”
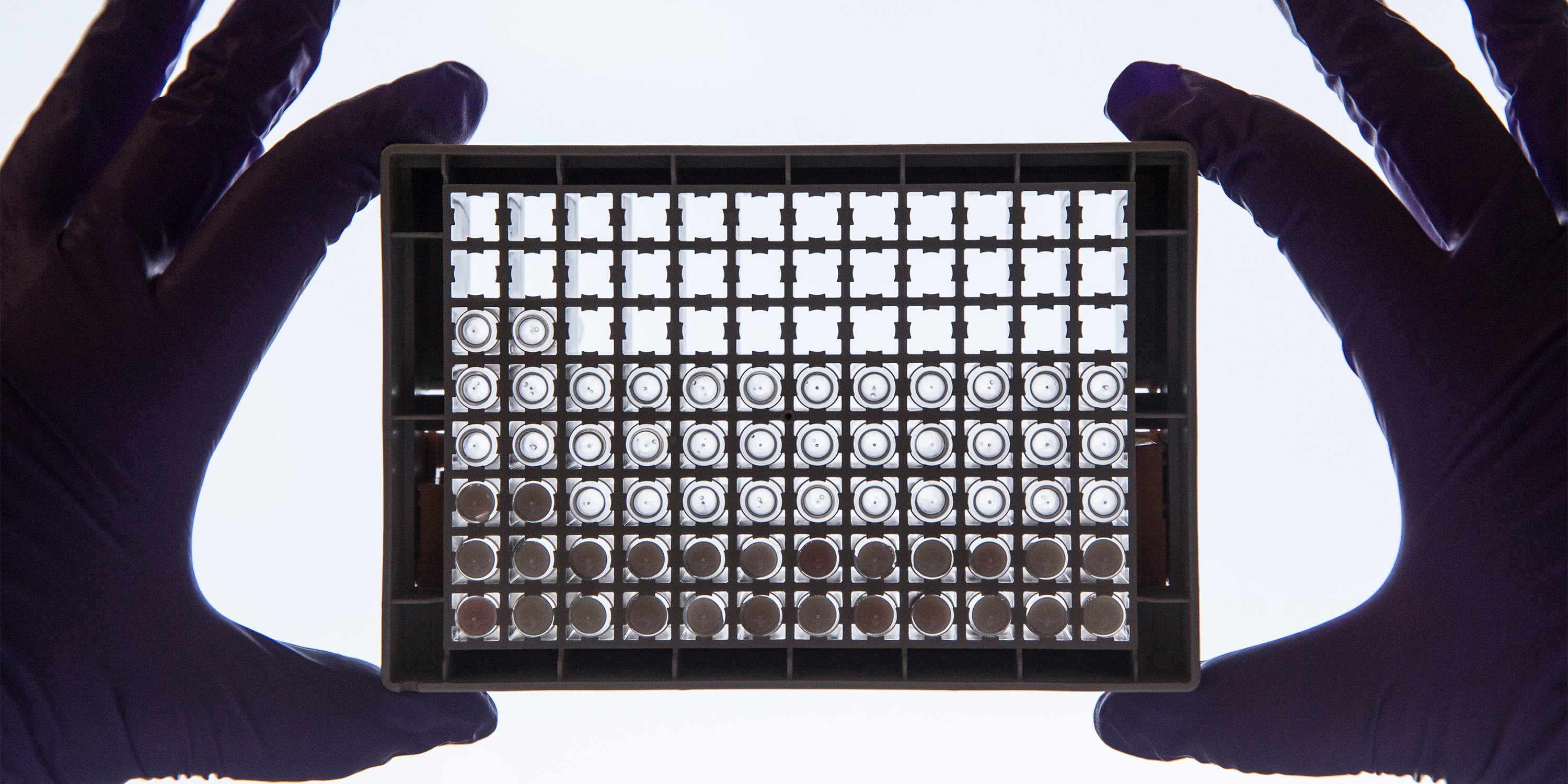
Drug delivery is an important area of research, as getting cancer drugs to where they are needed can be challenging.
“Using innovative methods, such as
“The preceding TarDox study here at the University of Oxford showed the potential for combining new treatment delivery techniques with chemotherapy, and we want to extend this to immunotherapies and in notoriously hard-to-treat cancers, like those in the pancreas.”
Against acute myeloid leukemia
In April 2021, Prof. Tony Kouzarides, from the Milner Therapeutics Institute and the Gurdon Institute at the University of Cambridge in the U.K., published the results of a new study.
In the paper, the authors outline a new drug class that might help treat acute myeloid leukemia (AML).
AML is a blood cancer in which bone marrow produces abnormal myeloid blood cells. These white blood cells normally protect the body against infection and the spread of tissue damage.
AML progresses rapidly, and, without treatment, it can be fatal within weeks or months. According to the American Cancer Society, AML was responsible for an estimated
Speaking with MNT, Prof. Kouzarides explained their approach:
“Proteins are essential for our bodies to function and are produced by a process that involves translating our DNA into RNA using enzymes. Sometimes, this process can go awry, with potentially devastating consequences for human health. Until now, no one has targeted this essential process as a way of fighting cancer.”
“We’ve identified a drug-like molecule, STM2457, that can inhibit the action of a key enzyme involved in the development and maintenance of AML.”
The enzyme in question is called METTL3. During AML, this enzyme becomes overexpressed in some cells, driving the condition onward.
“In tissue cultured from individuals with AML and in mouse models of the disease, we’ve shown that our drug is able to block the cancerous effect caused by overexpression of the enzyme.”
“This is a brand new field of research for cancer and the first drug-like molecule of its type to be developed — it’s the beginning of a new era for cancer therapeutics.”
Cancer research and CERN
MNT spoke with Prof. Thomas Elias Cocolios, from KU Leuven’s Department of Physics and Astronomy in Belgium. His cancer research takes place in what one might consider an unlikely venue: the European Organization for Nuclear Research (CERN).
His field of interest is nuclear medicine. In nuclear medicine, healthcare professionals introduce radioactive materials into the body. Known as radioisotopes or radiopharmaceuticals, these materials can help diagnose or treat cancer.
In diagnosis, nuclear medicine is useful in creating PET scans. As a treatment, people can swallow, inject, or inhale radiopharmaceuticals to treat certain types of cancer.
As Prof. Cocolios explained, nuclear medicine’s ability to both image and treat cancer provides substantial benefits.
“The targeted action of radiopharmaceuticals and their high specificity allow us to expose cancer cells throughout the body, and, with the appropriate combination of partner isotopes, switching from imaging to treatment guarantees that cancer cells are specifically targeted and healthy tissue is spared.”
This use of nuclear medicine to both diagnose and treat is known as theranostics.
However, advances in nuclear medicine have stalled. Prof. Cocolios told MNT that although nuclear physicists have produced more than 3,000 different isotopes, nuclear medicine has long been limited to just a “handful” of radioisotopes.
This, he explained, is primarily due to “a technical issue rather than a medical one: their limited supply.”
“No one will invest in producing a radioisotope [whose] action has not been extensively investigated; no one will investigate a radioisotope that is not reliably available: a vicious circle that ought to be broken.”
– Prof. Thomas Elias Cocolios
Prof. Cocolios works within the Medical Isotopes Collected from Isolde (MEDICIS) department at CERN.
This facility produces a range of radioisotopes for research into cancer diagnosis and treatment and sends them to partner university hospitals. Recipients include the Geneva University Hospital in Switzerland, the Lausanne University Hospital in Switzerland, and the UZ Leuven University Hospital in Belgium.
He told us how MEDICIS “uses a mass separation technique that allows [it] to produce carrier-free radioisotopes with very high specific activities, which are appropriate for nuclear medicine applications.”
As part of the European medical isotope program, this work is providing a stream of free radioisotopes to research teams across Europe.
Currently, MEDICIS is supporting preclinical work, so its radioisotope will not reach the clinic for some time. However, Prof. Cocolios is hopeful about the future.
CAR T in the spotlight
Dr. Joel Newman, a consultant hematologist and specialty lead for pathology at East Sussex Healthcare Trust in the U.K., is particularly excited about the future of a particular type of immunotherapy to treat hematological cancers: chimeric antigen receptor T (CAR T) cell therapies.
He explained to MNT: “We can now take lymphocytes from patients, program them to attack the relevant abnormal cell, and then reinfuse them — turning the patients’ own immune system against their cancer.”
This simplistic explanation belies the complexity of the task. As Dr. Newman explained, “At the moment, this is a relatively laborious task” because each patient’s cells need to be “trained.”
Currently, there are just
“In time, there will likely be ‘off-the-shelf’ treatments in this area that will continue to revolutionize cancer care,” said Dr. Newman.
New treatment, old target
We also contacted Dr. Helen Rippon, the chief executive of Worldwide Cancer Research. She is particularly excited about recent research into MYC proteins.
Dr. Rippon explained to MNT that “for a long time, MYC has been a promising cancer target because it drives tumor growth in 70% of all cancers.”
“But because of its location in the nucleus [of the cell] and because MYC is central to so many different mechanisms within the cell, scientists also feared that blocking it might cause catastrophic side effects. Some even called it ‘
The MYC protein plays a wide range of roles within the cell. It activates
Scientists feared that blocking MYC would not be a viable way to approach cancer treatment, as it would have too many knock-on effects.
However, experts may soon revoke MYC’s “undruggable” status. As Dr. Rippon told MNT, “One of the most exciting recent advances for us has been the launch of clinical trials for a brand new type of cancer treatment targeting MYC.”
“Spearheaded by the research of Dr. Laura Soucek, based at the Vall d’Hebron Institute of Oncology in Spain, the first ever drug targeting MYC is about to be tested in a clinical trial of 20 patients with varying types of advanced solid tumors.”
The drug, known as Omomyc, is a miniprotein that inhibits the work of MYC.
As Dr. Rippon told MNT, “Worldwide Cancer Research, a Scottish-based U.K. charity that starts cancer cures around the globe, funded Dr. Soucek back in 2013 to allow her to develop her new treatment and prove that it was ready for clinical trials.”
“It is incredibly exciting to see how ingenuity and perseverance [have] allowed for a promising new treatment that once was thought to be impossible to enter clinical trials.”
Dr. Soucek has been working on MYC inhibitors for more than 20 years. Early studies in mice produced encouraging results, but at that stage, Omomyc was only available as a gene therapy. Although gene therapy holds promise, it is not yet ready for use in patients.
Many scientists believed that Omomyc would be too bulky as a drug and that it would not be able to enter the cell, let alone the nucleus where MYC resides.
In spite of these challenges, Dr. Soucek persevered, and despite the naysayers, she has created an Omomyc drug molecule that is now entering human trials.
Summary
Cancer research moves fast. Scientists are tackling the many problems associated with cancer from a range of different angles.
Although we have only scratched the surface in this feature, it is clear that there are many reasons to be hopeful.

