Multiple sclerosis (MS) is a chronic disease that affects the central nervous system, including the brain, spinal cord, and optic nerves. Symptoms can range from muscle weakness to vision loss. They tend to worsen during flares and improve during times of remission.
It is not possible to predict how multiple sclerosis (MS) will progress in any individual.
Some people have mild symptoms, such as blurred vision and numbness, and tingling in the limbs. In severe cases, a person may experience paralysis, vision loss, and mobility problems. However, this is not common.
It is difficult to know precisely how many people have MS. According to the National Institute for Neurological Disorders and Stroke (NINDS),
The National Multiple Sclerosis Society estimates the number could be closer to 1 million.
New treatments are proving effective at slowing the disease.

Scientists do not know exactly what causes MS, but
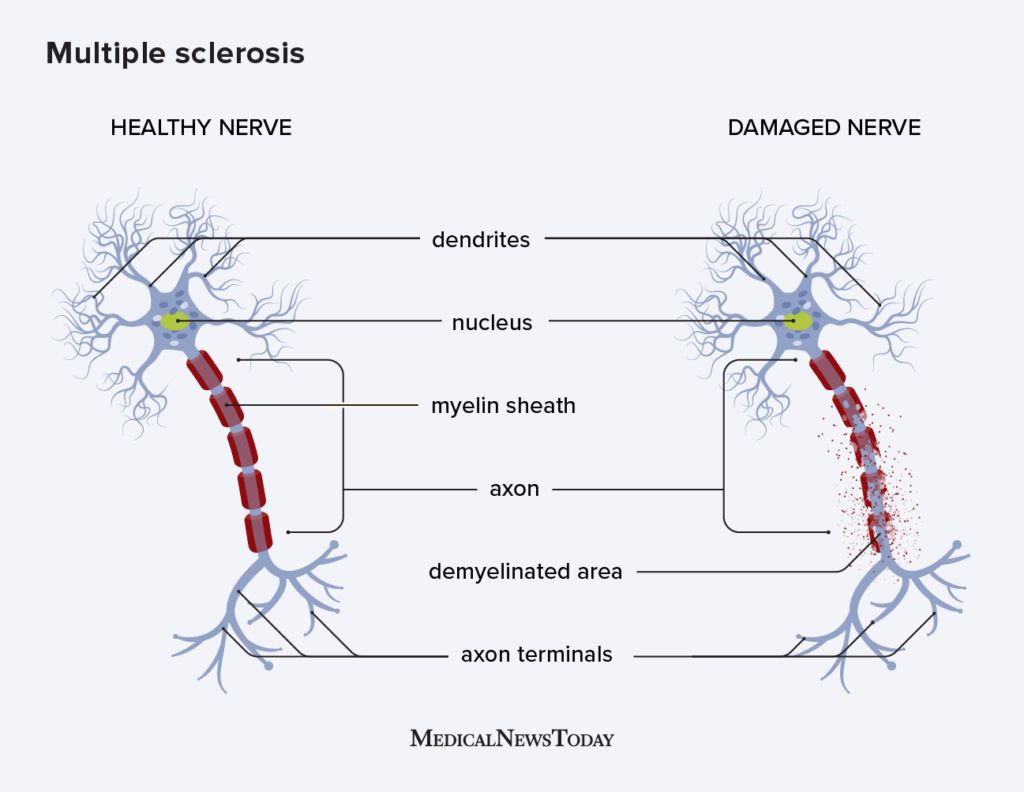
In the case of MS, the immune system attacks the myelin sheath that surrounds and protects the nerve fibers, causing inflammation. Myelin allows the nerves to conduct electrical signals quickly and efficiently.
Multiple sclerosis means “scar tissue in multiple areas.”
When the myelin sheath disappears or sustains damage in multiple areas, it leaves a scar, or sclerosis. Doctors also call these areas plaques or lesions. They mainly affect:
- the brain stem
- the cerebellum, which coordinates movement and controls balance
- the spinal cord
- the optic nerves
- white matter in some regions of the brain
As more lesions develop, nerve fibers can break or become damaged. As a result, the electrical impulses from the brain do not flow smoothly to the target nerve. This means that the body cannot carry out certain functions.
There are four types of MS:
Clinically isolated syndrome (CIS)
This is a single, first episode, with symptoms lasting at least 24 hours. If another episode occurs at a later date, a doctor might diagnose relapse-remitting MS.
Relapse-remitting MS (RRMS)
This is the most common form. Around 85% of people with MS are initially diagnosed with RRMS. RRMS involves episodes of new or increasing symptoms, followed by periods of remission, during which symptoms go away partially or totally.
Primary progressive MS (PPMS)
Symptoms worsen progressively without early relapses or remissions. Some people may experience times of stability and periods when symptoms worsen and then get better. Around 15% of people with MS have PPMS.
Secondary progressive MS (SPMS)
At first, people will experience episodes of relapse and remission, but then the disease will start to progress steadily.
Find out more here about the different types and multiple sclerosis stages and what they mean.
Because MS affects the CNS, which controls all the actions in the body, symptoms can affect any part of the body.
The most common symptoms of MS are:
- Muscle weakness: People may develop weak muscles due to lack of use or stimulation due to nerve damage.
- Numbness and tingling: A pins and needles-type sensation is one of the earliest symptoms of MS and can affect the face, body, arms, and legs.
- Lhermitte’s sign: A person may experience a sensation like an electric shock when they move their neck, known as Lhermitte’s sign.
- Bladder problems: A person may have difficulty emptying their bladder or need to urinate frequently or suddenly, known as urge incontinence. Loss of bladder control is an early sign of MS.
- Bowel problems: Constipation can cause fecal impaction, which can lead to bowel incontinence.
- Fatigue: Fatigue can undermine a person’s ability to function at work or at home, and is one of the most common symptoms of MS.
- Dizziness and vertigo: These are common problems, along with balance and coordination issues.
- Sexual dysfunction: Both males and females may lose interest in sex.
- Spasticity and muscle spasms: This is an early sign of MS. Damage to nerve fibers in the spinal cord and brain can cause painful muscle spasms, including in the legs.
- Tremor: Some people with MS may experience involuntary quivering movements.
- Vision problems: Some people may experience double or blurred vision or a partial or total loss of vision. This usually affects one eye at a time. Inflammation of the optic nerve can result in pain when the eye moves. Vision problems are an early sign of MS.
- Gait and mobility changes: MS can change the way people walk due to muscle weakness and problems with balance, dizziness, and fatigue.
- Emotional changes and depression: Demyelination and nerve fiber damage in the brain can trigger emotional changes.
- Learning and memory problems: These can make it difficult to concentrate, plan, learn, prioritize, and multitask.
- Pain: Pain is a common symptom in MS. Neuropathic pain is directly due to MS, while muscle spasticity or stiffness may cause localized pain.
Less common symptoms include:
- headaches
- hearing loss
- itching
- respiratory or breathing problems
- seizures
- speech disorders
- swallowing problems
There is also a higher risk of urinary tract infections, reduced activity, and loss of mobility. These can impact a person’s work and social life.
In the later stages, people may experience changes in perception and thinking, as well as sensitivity to heat.
MS affects individuals differently. For some, it starts with a subtle sensation, and their symptoms do not progress for months or years. Sometimes, symptoms worsen rapidly, within weeks or months.
A few people will only have mild symptoms, and others will experience significant changes that lead to disability. However, most people will experience times when symptoms worsen and then get better.
Scientists do not really know what causes MS, but
- Age: Most people receive a diagnosis between the ages of 20 and 40 years.
- Sex: Most forms of MS are twice as likely to affect women than men.
- Genetic factors: Susceptibility may pass down in the genes, but scientists believe an environmental trigger is also necessary for MS to develop, even in people with specific genetic features.
- Smoking: People who smoke appear to be more likely to develop MS. They also tend to have more lesions and brain shrinkage than non-smokers.
- Infections: Exposure to viruses, such as Epstein-Barr virus (EBV) or mononucleosis,
may increase a person’s risk of developing MS, but research has not shown a definite link. Other viruses that may play a role include human herpes virus type 6 (HHV6) and mycoplasma pneumonia. - Vitamin D deficiency: MS is more common among people who have less exposure to bright sunlight, which is necessary for the body to create vitamin D. Some experts think that low levels of vitamin D may affect the way the immune system works.
- Vitamin B12 deficiency: The body uses vitamin B when it produces myelin. A lack of this vitamin
may increase the risk of neurological diseases such as MS.
Previous theories have included exposure to canine distemper, physical trauma, or aspartame, an artificial sweetener, but there is no evidence to support these. There is probably no single trigger for MS, and it is likely that multiple factors will contribute to its occurrence.
A doctor will carry out a physical and neurological examination, ask about symptoms, and consider the person’s medical history.
No single test can confirm a diagnosis, so a doctor will use several strategies when deciding whether a person meets the criteria for a diagnosis.
These include:
- MRI scans of the brain and spinal cord, which may reveal lesions
- spinal fluid analysis, which may identify antibodies that suggest a previous infection or proteins consistent with a diagnosis of MS
- an evoked potential test, which measures electrical activity in response to stimuli
Other conditions have symptoms that are similar to those of MS, so a doctor may suggest other tests to assess for other possible causes of the person’s symptoms.
If the doctor diagnoses MS, they will need to identify what type it is and whether it is active or not. The person may need more tests in the future to check for further changes.
There is no cure for MS, but treatment is available that can slow the progression of the disease, reduce the number and severity of relapses, and relieve symptoms.
Some people also use complementary and alternative therapies, but research does not always confirm the usefulness of these.
Treatment options include:
Medications to slow progression
Several
A doctor may give some of these by mouth, by injection, or as an infusion. How often the person needs to take them and whether they can do this at home will depend on the drug.
The following DMTs currently have FDA approval:
Injectable medications
- Avonex (interferon beta-1a)
- Betaseron (interferon beta-1b)
- Copaxone (glatiramer acetate)
- Extavia (interferon beta-1b)
- Glatiramer Acetate Injection (glatiramer acetate — generic equivalent of Copaxone 20 mg and 40 mg doses)
- Glatopa (glatiramer acetate — generic equivalent of Copaxone 20mg and 40mg doses)
- Kesimpta (ofatumumab)
- Plegridy (peginterferon beta-1a)
- Rebif (interferon beta-1a)
Oral medications
- Aubagio (teriflunomide)
- Bafiertam (monomethyl fumarate)
- Dimethyl Fumarate (dimethyl fumarate — generic equivalent of Tecfidera)
- Gilenya (fingolimod)
- Mavenclad (cladribine)
- Mayzent (siponimod)
- Ponvory (ponesimod)
- Tecfidera (dimethyl fumarate)
- Vumerity (diroximel fumarate)
- Zeposia (ozanimod)
Infused medications
- Lemtrada (alemtuzumab)
- Novantrone (mitoxantrone)
- Ocrevus (ocrelizumab)
- Tysabri (natalizumab)
Current guidelines recommend a person begin using these drugs when in the early stages of MS, as there is a good chance that they can slow the progression of MS, especially if the person takes them when symptoms are not yet severe.
Doctors
Adverse effects of immunosuppressant drugs include a higher risk of infections. Some medications may also harm the liver. If a person notices adverse effects or if their symptoms worsen, they should seek medical advice.
Relieving symptoms during a flare
Other drugs are useful when a person experiences a worsening of symptoms during a flare. They will not need these drugs all the time.
These medications include corticosteroids, which reduce inflammation and suppress the immune system. They can treat an acute flare-up of symptoms in certain types of MS. Examples include Solu-Medrol (methylprednisolone) and Deltasone (prednisone). Steroids can have adverse effects if a person uses them too often, and they are not likely to provide any long-term benefit.
Other medications and approaches can treat specific symptoms. Those symptoms include:
- Behavioral changes: If a person has vision problems, a doctor may recommend they rest their eyes from time to time or limit screen time. A person with MS may need to learn to rest when fatigue sets in and to pace themselves so they can complete activities.
- Problems with mobility and balance: Physical therapy and walking devices, such as a cane, may help. The drug dalfampridine (Ampyra) may also prove useful.
- Tremor: A person may use assistive devices or attach weights to their limbs to reduce shaking. Medications may also help with tremors.
- Fatigue: Getting enough rest and avoiding heat can help. Physical and occupational therapy can help teach people more comfortable ways to do things. Assistive devices, such as a mobility scooter, can help conserve energy. Medication or counseling may help boost energy by improving sleep.
- Pain: Pain relief medication, such as gabapentin, may help with body pain. Doctors may also prescribe muscle relaxants to reduce painful spasms.
- Bladder and bowel problems: Some medications and dietary changes can help resolve these issues.
- Depression: A doctor may prescribe a selective serotonin reuptake inhibitor (SSRI) or other antidepressant drugs.
- Cognitive changes: Donepezil, a drug for Alzheimer’s, may help some people.
Learn more here about how to manage an exacerbation of MS.
Complementary and alternative therapies
The following may help with different aspects of MS:
- heat and massage treatment for pain
- acupuncture for pain and gait
- stress management to boost mood
- exercise to maintain strength and flexibility, reduce stiffness, and boost mood
- a healthful diet with plenty of fresh fruits, vegetables, and fiber
- quitting or avoiding smoking
What is a healthful diet for a person with MS? Find out here.
Medical cannabis
Cannabis-based treatments may help relieve pain, muscle stiffness, and insomnia. However, there is not enough evidence to confirm this.
People considering this approach should note that there is a difference between using street cannabis and medical cannabis. Also, not all forms of cannabis are legal in all states.
A person should ask their doctor for advice before using cannabis, as some forms can have adverse effects. Smoking cannabis is unlikely to be beneficial, and it may make symptoms worse.
Some people have suggested that biotin may help. Find out more here.
Rehabilitation and physical therapy
Rehabilitation can help improve or maintain a person’s ability to perform effectively at home and work.
Programs generally include:
- Physical therapy: This aims to provide the skills to maintain and restore maximum movement and functional ability.
- Occupational therapy: The therapeutic use of work, self-care, and play may help maintain mental and physical function.
- Speech and swallowing therapy: A speech and language therapist will carry out specialized training for those who need it.
- Cognitive rehabilitation: This helps people manage specific problems in thinking and perception.
- Vocational rehabilitation: This helps a person whose life has changed with MS make career plans, learn job skills, and get and keep a job.
Plasma exchange
This process removes the antibodies in the blood that are attacking parts of the person’s body, but whether it can help people with MS is unclear. Studies have produced mixed results.
Plasma exchange is usually only suitable for severe MS attacks.
Stem cell therapy
Scientists are looking into the use of
Researchers hope that one day, stem cell therapy techniques may be able to reverse the damage done by MS and restore functionality in the nervous system.
MS is challenging to live with but is rarely fatal. Some severe complications such as bladder infections, chest infections, and difficulty swallowing could lead to death.
A multiple sclerosis prognosis does not always result in severe paralysis. Two-thirds of people with MS are able to walk. However, many of them will require assistance such as a cane, wheelchair, crutches, or a scooter.
The average life expectancy for a person with MS is 5 to 10 years lower than the average person.
Here are some frequently asked questions about MS.
How does someone cope with MS?
MS presents psychological and emotional challenges. The National Multiple Sclerosis Society suggests the following tips for coping:
- reduce and manage stress, such as with meditation or journaling
- focus on the positive
- view challenges as opportunities for creative problem solving
- foster and nurture relationships with others
- share coping methods with family members
Can someone live a normal life with MS?
MS can cause unique challenges and health complications that may cause someone to require lifestyle modifications and adjustments.
This may include walking aids and ongoing treatment, including medication and therapy to manage changes, such as cognitive or vocational rehabilitation.
What is the average life expectancy with MS?
Life expectancy for a person with MS is around 5–10 years lower than average, according to the UK’s National Health Service.
However, every person’s outlook will be different. A person’s doctor can provide them with more accurate information about life expectancy.
Is MS treatable if people catch it early?
There is no cure for MS. However, early treatment can help to slow disease progression, relieve symptoms, and reduce the severity of relapses.
MS is a potentially severe health condition that affects the nervous system. Progression of MS is different for each person, so it is hard to predict what will happen, but most people will not experience severe disability.
In recent years, scientists have made rapid progress in developing drugs and treatments for MS. Newer drugs are safer and more effective, and they offer significant hope for slowing disease progression.
As researchers learn more about genetic features and changes that occur with MS, there is also hope that they will be able to predict more easily which kind of MS a person will have and establish the most effective treatment from the earliest stage.
A person who receives appropriate treatment and follows a healthful lifestyle can expect to live the
It is important to have support from people who understand what it is like to receive a diagnosis of and live with MS. MS Healthline is a free app that provides support through one-on-one conversations and live group discussions with people who have the condition. Download the app for iPhone or Android.
